How to Determine Whether Your Pregnancy Is Viable or Nonviable

- What Is a Viable Pregnancy?
- How Is Viable Pregnancy Determined?
- What Is a Nonviable Pregnancy?
- Causes of Nonviable Pregnancy
- Symptoms of Nonviable Pregnancy
- How Is Nonviable Pregnancy Determined?
- Management Options for Nonviable Pregnancy
- How to Cope With Nonviable Pregnancy?
- FAQs
Pregnancy is one such phase in a woman’s life when no amount of information seems enough. All the smiles that brightened the faces of pregnant women and their families are soon replaced by worry and concerns about pregnancy, nursing and parenthood. One such question that doesn’t miss a single pregnant lady is whether their pregnancy is viable or not. In this article, we shall talk about what viable and nonviable pregnancies are and the aspects that lead to them.
Although the concept of viable and nonviable pregnancy is easy to grasp, the definitions are clearer in the medical world. To explain it in a few words, a viable pregnancy is when the baby is developing well and has a reasonable chance to make it to the full term, while a nonviable pregnancy is when a baby has no chance of being born alive. Read on to know more including how many weeks is a pregnancy viable.
What Is a Viable Pregnancy?
A viable pregnancy denotes that the foetus is alive and the pregnancy is progressing normally. Before the foetal heartbeat is detected, viable could just mean that the pregnancy hormone hCG is rising the way it should. When there is a foetus in the uterus, and it shows up in ultrasound with a healthy heart rate and normal development, the doctors would call it a viable intrauterine pregnancy.
How Is Viable Pregnancy Determined?
There are several hints that help determine whether a pregnancy is viable. Here are some of them:
1. Human Chorionic Gonadotropin (HCG) Hormone
The HCG is a hormone produced by the placenta during its implantation process in the uterus. During a normal pregnancy, the levels of the HCG hormone steadily increase over the days. Home pregnancy test kits measure HCG levels in the urine, but a blood test would give an exact reading. Four weeks into the pregnancy, the HCG levels would range between 17 to 119 mIU/ml. What’s important to know however, is that it’s not the number that counts, it is whether the number doubles every two or three days. In over 85% of normal pregnancies, the HCG levels double and once it reaches 2000 mIU/ml, some embryonic development becomes apparent on the transvaginal ultrasound.
2. Gestational Sac
When a woman is four weeks pregnant, the embryo gets implanted in the uterus. This is when the first pregnancy test reads positive, and at four weeks, there’s still nothing that can be picked up by an ultrasound scan. By the next week, the gestational sac, the sac that holds the developing embryo, comes into view. By six weeks, a yolk sac can be seen within the gestational sac in an ultrasound. The yolk sac gives nutrition to the embryo before the placenta is developed. Post the development of the yolk sac, the images of an embryo can be obtained via ultrasound scans. If the embryo has a heartbeat, it suggests that the pregnancy is progressing as usual.
3. Foetal Pole
When the embryo begins developing, it looks more like a small bean, with a tiny straight pole that is curved a little at the tail. The foetal pole develops around five-and-a-half to six-and-a-half weeks of pregnancy. It is measured from the head (crown) and the bottom of the buttocks (rump). This length is called the crown-rump length (CRL), and taking its measurement is important because once the CRL of the foetus exceeds 7mm, a heartbeat should be detected through a transvaginal ultrasound. The presence of a heartbeat suggests a healthy progressing pregnancy.

4. Foetal Heartbeat
When the foetal heartbeat first becomes detectable, the heart is still a tiny one-chambered tube. The heartbeat appears as a little flicker on the ultrasound scan at around six weeks, which is an indicator of a healthy foetus. The heart rate is initially slower, and once the foetus develops a full heart with four chambers, the heartbeat is around 110 beats per minute (BPM) in a viable intrauterine pregnancy. However, a foetal heart rate of less than 90 beats per minute might indicate a nonviable pregnancy. A healthy heart rate is an indicator of a viable pregnancy, and once it is seen, the chance of a miscarriage drops significantly and about 95% of the pregnancies from this stage go on to be full term.
5. Symptoms of Pregnancy
Early pregnancy symptoms are normally an indicator that the pregnancy is developing normally. Many women wonder if morning sickness is a good sign of a viable pregnancy and the answer is that there is a good chance it could be so when coupled with other signs such as nausea, sore breasts, frequent urination and fatigue. These symptoms result due to varying pregnancy hormones in the body.
What Is a Nonviable Pregnancy?
A nonviable pregnancy is when there is no chance of a live infant being born out of the pregnancy, or the foetus does not have a chance to survive even when born alive. Diagnostically, in the early stages, nonviable does not mean that the foetus has a little chance of survival; it has no chances of survival. In the early stages of gestation, it is possible to experience a nonviable pregnancy, but no miscarriage. However, the symptoms of miscarriage show up eventually.
Causes of Nonviable Pregnancy
In a nonviable pregnancy, the foetus has no chance of survival, and there are many reasons why that might be so. Here are the most common ones:
- It could be an ectopic pregnancy where the fertilized egg gets implanted outside of the uterus, such as the fallopian tubes.
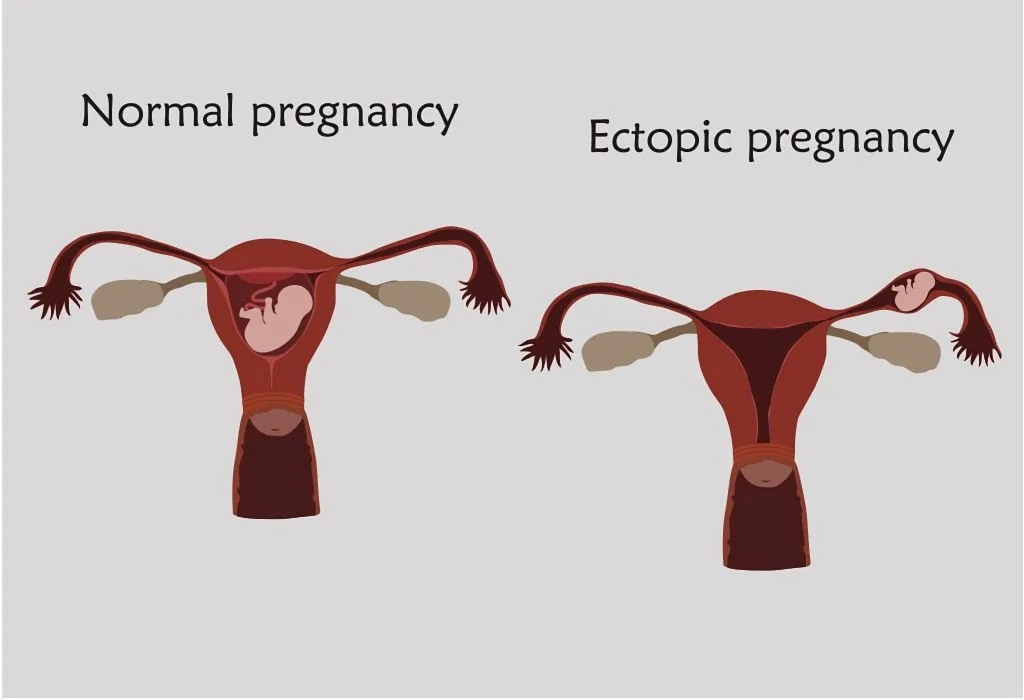
- Molar pregnancy is an abnormal form of pregnancy in which a non-viable fertilized egg implants in the uterus and will fail to come to term. A molar pregnancy is a gestational trophoblastic disease which grows into a mass in the uterus
- A chemical pregnancy also results in a nonviable pregnancy when the fertilized egg fails to implant in the uterus.
- An anembryonic gestation which is also known as blighted ovum is another condition wherein the pregnancy stops after the gestational sac forms.
- Pregnancies where the foetus no longer has a heartbeat.
- Congenital defects which make survival impossible for the foetus.
- A premature birth when the baby is unable to survive.
Symptoms of Nonviable Pregnancy
A nonviable pregnancy refers to a pregnancy that is unable to progress and results in the birth of a viable baby. It can be a distressing experience for individuals and couples hoping to conceive. Recognizing the following signs of a non-viable pregnancy is crucial for seeking appropriate medical care and support.
- Vaginal bleeding or spotting: This can range from light spotting to heavy bleeding and may be accompanied by abdominal cramping.
- Absence of fetal heartbeat: During prenatal check-ups, the absence of a fetal heartbeat on ultrasound can indicate a nonviable pregnancy.
- Decreasing or plateauing levels of human chorionic gonadotropin (hCG): HCG levels typically rise during early pregnancy but may plateau or decrease in a nonviable pregnancy.
- Lack of fetal growth: Ultrasound examinations may reveal that the fetus is not growing as expected or has stopped growing altogether.
- Absence of fetal movement: In later stages of pregnancy, the absence of fetal movement despite fetal viability can be indicative of a nonviable pregnancy.
How Is Nonviable Pregnancy Determined?
The Society of Radiologists in Ultrasound (SRU) has a definite set of criteria which is used to determine if a pregnancy is nonviable. Here are some of them.
- The CRL is 7 mm or more with no heartbeat in the foetus.
- The gestational sac has a mean diameter of 25 mm or more but has no embryo in it.
- Absence of the yolk sac in the gestational sac in the first scan, and two or more weeks later, there is no embryo with a heartbeat.
- Gestational sac with a yolk sac is seen in the scan, but 11 or more days later there is no embryo with a heartbeat.
- CRL length is less than 7 mm without a heartbeat.
- Gestational sac diameter between 10 to 24 mm and no embryo.
- There is no embryo 6 or more weeks after the last menstrual period.
- The amnion (the membrane that surrounds the embryo) is absent.
- Enlarged yolk sac that is bigger than 7 mm.
- The size of the gestational sac is comparatively smaller than the embryo
Management Options for Nonviable Pregnancy
When faced with a nonviable pregnancy, individuals and couples may need to consider management options that prioritize their physical and emotional well-being while addressing the situation with care and compassion.
1. Expectant Management
This approach involves allowing the body to naturally expel the nonviable pregnancy without medical intervention. It may be suitable for individuals who prefer a more conservative approach and are willing to wait for the body to initiate the miscarriage process spontaneously.
2. Medical Management
In some cases, healthcare providers may prescribe medications, such as misoprostol, to help induce the miscarriage and facilitate the expulsion of pregnancy tissue. Medical management may be preferred by individuals who desire a more controlled and predictable process or who are experiencing complications that necessitate intervention.
3. Surgical Management
Surgical options, such as dilation and curettage (D&C) or dilation and evacuation (D&E), involve the removal of pregnancy tissue from the uterus under anesthesia. Surgical management may be recommended for individuals experiencing excessive bleeding, incomplete miscarriage, or signs of infection, or for those who prefer a more expedited resolution.
4. Emotional Support and Counseling
Regardless of the chosen management option, receiving emotional support and counseling is essential for individuals and couples navigating a nonviable pregnancy. Support groups, counseling services, and resources provided by healthcare professionals can help individuals cope with grief, loss, and the emotional challenges associated with pregnancy loss.
How to Cope With Nonviable Pregnancy?
After experiencing a nonviable pregnancy, it’s important not only to address any physical recuperation necessary but also to focus on emotional healing. Dealing with the loss of a pregnancy can have significant effects and may necessitate nurturing your mental well-being. Allowing yourself the space and time to mourn is crucial. Finding a supportive individual to confide in, whether it’s a partner, family member, close friend, or therapist, can provide solace and aid in the healing process.
FAQs
1. What is a non-viable birth?
A non-viable birth refers to the spontaneous loss of a fetus before reaching 20 weeks of gestation, as confirmed by a healthcare provider.
2. Is it possible that the non-viable pregnancy be misdiagnosed?
Yes, it’s possible for a non-viable pregnancy to be misdiagnosed, especially in the early stages. Follow-up evaluations may be needed for confirmation.
3. Can HCG levels increase in pregnancies that are not viable?
In some cases, HCG levels may increase initially in non-viable pregnancies, but they typically either plateau or decrease over time.
4. How much time does it usually take for the body to naturally expel a pregnancy that is not viable?
The time it takes for the body to naturally expel a non-viable pregnancy can vary. It may occur within a few days to a few weeks.
5. How long should a woman wait before attempting to conceive again after a non-viable pregnancy?
When it’s not a viable pregnancy, it’s recommended for a woman to wait until she has physically and emotionally recovered before attempting to conceive again. This timeframe varies for each individual but may range from a few weeks to several months. Consulting with a healthcare provider is advisable for personalized guidance.
We hope you found this information on viable and non-viable pregnancies helpful!
References/Resources:
1. Breborowicz. G; Limits of fetal viability and its enhancement (Early Pregnancy); National Library of Medicine; https://pubmed.ncbi.nlm.nih.gov/11753511/; January 2001
2. The Science of Viability (Later Abortion Initiative); Ibis Reproductive Health; https://laterabortion.org/sites/default/files/lai_factsheet_viability.pdf; April 2018
3. Doubilet. P, Benson. C, Bourne. T, Blaivas. M; Diagnostic Criteria for Nonviable Pregnancy Early in the First Trimester; The New England Journal of Medicine; https://geiselmed.dartmouth.edu/radiology/wp-content/uploads/sites/47/2019/04/Non-viable-pregnancy.pdf
4. Schreiber. C, Sammel. M, Hillier. S, Barnhart. K; A Little Bit Pregnant: Modeling How the Accurate Detection of Pregnancy Can Improve HIV Prevention Trials (American Journal of Epidemiology); National Library of Medicine; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2732971/; February 2009
5. Molar Pregnancy; Penn Medicine Lancaster General Health; https://www.lancastergeneralhealth.org/healthwise-library/healthwise-article?documentId=hw165877
6. Understanding Blighted Ovum; UC San Diego Health; https://myhealth.ucsd.edu/Spanish/RelatedItems/3,90761
7. Pelvic Ultrasound: What to Expect; University of Michigan; https://www.med.umich.edu/1libr/radiology/NuclearMedicinePreps/PelvicUS.pdf
Also Read:
Heterotopic Pregnancy
Causes of Molar Pregnancy
Symptoms of Abdominal Pregnancy
Was This Article Helpful?
Parenting is a huge responsibility, for you as a caregiver, but also for us as a parenting content platform. We understand that and take our responsibility of creating credible content seriously. FirstCry Parenting articles are written and published only after extensive research using factually sound references to deliver quality content that is accurate, validated by experts, and completely reliable. To understand how we go about creating content that is credible, read our editorial policy here.