Chemical Pregnancy: Causes, Symptoms, and Treatments

A chemical pregnancy is a term used for a condition where an early miscarriage occurs within the first five weeks of pregnancy. It accounts for 50% to 70% of all miscarriages and is characterised by heavy bleeding close to the time of your expected period after receiving a positive pregnancy test. The test may indicate a positive result, but soon after, the pregnancy hormones drop, leading to miscarriage. Read on to recognise the symptoms of a chemical pregnancy and how to deal with one if it happens to you.
What Is a Chemical Pregnancy?
Let’s take a look at the chemical pregnancy definition. A chemical pregnancy is a very early miscarriage that occurs shortly after implantation. It is not a false positive or a false pregnancy on a pregnancy test but a proper pregnancy that ends in a miscarriage. Although the term seems like a misnomer, it is referred to as a chemical pregnancy due to the time that it takes place. Chemical pregnancies occur at an early time during the pregnancy, where only a chemical pregnancy test is able to confirm the pregnancy. During this initial phase, not even an ultrasound scan can detect it, and only a biochemical test can tell if the woman is pregnant. Contrary to the general notion, chemical pregnancies are quite common, and unless tested positive for pregnancy, many women don’t realise they have had one.
How Common Is a Chemical Pregnancy?
Chemical pregnancy is surprisingly common, accounting for about 50% to 70% of all miscarriages. Many women may not even be aware they have experienced a chemical pregnancy because it typically occurs early in the first few weeks of pregnancy. Since the miscarriage happens so soon after a positive pregnancy test, many women might only experience a short-lived confirmation of pregnancy before symptoms of a miscarriage begin, often resembling a regular period. Regarding the chances of chemical pregnancy, it’s believed that chemical pregnancies can occur in up to 1 in 5 pregnancies, but because they are so early, they often go unnoticed.
Causes of Chemical Pregnancy
There could be several reasons for a chemical pregnancy to occur, and medical evidence is insufficient to determine what exactly causes it. However, it is known that abnormalities in the chromosomes of the developing foetus are a major cause of miscarriages, and the same applies to chemical pregnancies. Chromosomal abnormalities can occur due to various reasons, such as poor quality of the sperm or the egg, abnormalities in the genes that get passed on to the baby from one or both parents, and even abnormalities during cell division in the embryo. The general consensus in the medical community is that chromosomal abnormalities cause nearly half of all chemical pregnancies. Other factors that can cause chemical pregnancies include:
- Implantation of the foetus outside the uterus
- Hormonal imbalances and abnormalities
- Inadequate lining of the uterus
- Congenital or acquired abnormalities of the uterus
- Infections like syphilis, chlamydia, toxoplasmosis, etc.
- Uterine fibroids
- Few systemic diseases such as thyroid disease that is left untreated for a long time
- Blighted ovum
- Luteal phase defect– This is a condition where the abnormal positioning of the uterus inhibits the implantation.
Signs & Symptoms of a Chemical Pregnancy
At an early stage, chemical pregnancies usually go unnoticed as they are similar to the monthly periods. However, women who are trying to conceive and are tracking their ovulation can notice the changes that indicate a chemical pregnancy. Also, a chemical pregnancy after an IVF is a good sign that the woman can get pregnant, and further attempts could be successful.
- A pregnancy test at home that shows positive, which is followed by a heavier than normal period.
- Pain in the abdomen and more cramps
- Passing more clots than usual
- Delay in periods, especially if you get your periods regularly
- A light period, especially if you normally have it heavy
- Lowering of the hCG levels in the blood.
What Is the Difference Between a Chemical Pregnancy and a Miscarriage?
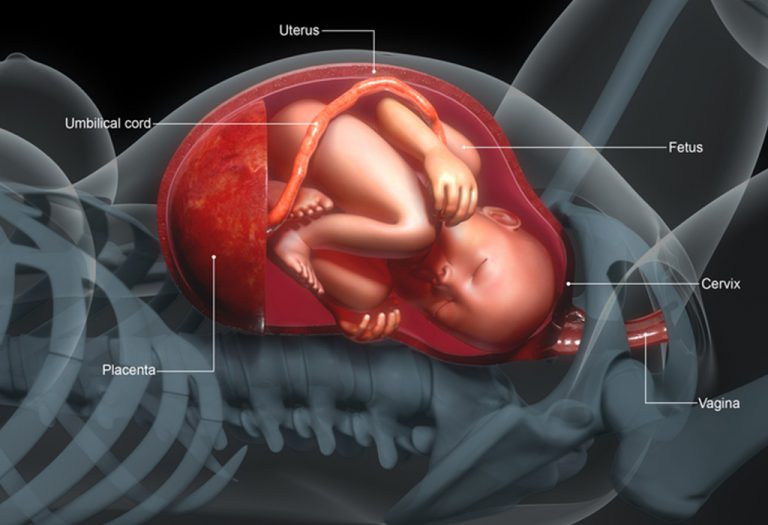
Fundamentally, a chemical pregnancy and a miscarriage is the same thing; the only difference between the two is the time of loss. They are both losses of a pregnancy but occur at different stages in the baby’s development. When a woman has a miscarriage after conception, but before the foetus has begun to develop, it is called a chemical pregnancy. The time typically is around three to four weeks when the woman’s body is producing enough hCG to give a positive pregnancy test. At this time a gestational sac or placenta hasn’t begun developing yet to be detected by an ultrasound scan. Hence the term chemical, as the pregnancy is only confirmed by a chemical test. Doctors would call a pregnancy loss after six weeks or more a miscarriage, as an ultrasound scan can detect the foetus.
Chemical Vs Clinical Pregnancy
A chemical pregnancy refers to an early miscarriage that occurs shortly after implantation, typically within the first five weeks of pregnancy. It is often identified through a positive pregnancy test, followed by heavy bleeding resembling a period due to a rapid drop in pregnancy hormones. Chemical pregnancies usually don’t show up on an ultrasound and are often diagnosed based on hormone levels or after a missed period.
In contrast, a clinical pregnancy is a pregnancy where the embryo is visible via ultrasound and the pregnancy progresses beyond the early stages. It typically involves the detection of a heartbeat and the growth of the fetus as confirmed through medical imaging. Clinical pregnancies generally continue beyond the early weeks, and any miscarriage that occurs would typically happen after the first trimester.
The key difference between the two lies in the stage of pregnancy when the miscarriage occurs: chemical pregnancies happen very early, often before the fetus is visible, while clinical pregnancies involve a more established pregnancy that can be monitored and diagnosed through medical means.
Risks of a Chemical Pregnancy
A chemical pregnancy, although common, can come with certain risks that may affect future pregnancies or overall reproductive health. Here are some potential risks associated with chemical pregnancies:
- Increased Risk of Future Miscarriages: Women who experience a chemical pregnancy may face a slightly higher risk of future miscarriages, although many go on to have healthy pregnancies later on.
- Hormonal Imbalances: A chemical pregnancy can sometimes be a sign of underlying hormonal imbalances, such as low progesterone or thyroid issues, which could affect future pregnancies.
- Emotional Impact: The emotional toll of experiencing a chemical pregnancy can be significant, as it often involves the loss of an early pregnancy that was initially confirmed with a positive test.
- Difficulties with Conception: In rare cases, a chemical pregnancy might indicate that there are challenges in conceiving or carrying a pregnancy to term, requiring further investigation and possible fertility treatments.
What Happens During a Chemical Pregnancy?
The fertilised egg takes about 6 to 12 days on an average to implant itself in the uterus. At about this time, the cells in the uterus that would later develop into the placenta, begin to produce the hormone hCG in amounts that can be detected in a home pregnancy test. It is still too early to detect the embryo or the gestational sac with an ultrasound, but the pregnancy is positive. After this stage, several factors can lead to the loss of pregnancy with one of the major factors being the health of the embryo. During conception, the sperm cell fertilises the egg to form a single-celled embryo called a zygote. The zygote begins to grow by cell division, and during this process, sometimes mistakes and abnormalities occur in the copying of the chromosomes. This process is random and can happen to anyone and is thought to be behind most of the losses at this stage.
Diagnosis
It is a chemical pregnancy when you test positive for pregnancy, and experience heavy bleeding and menstrual-like cramps afterwards. Consulting a doctor is imperative at this point as ectopic pregnancies also have similar characteristics and can be dangerous.
Treatment
There are no specific methods for treatment of chemical pregnancies; however, there are a few tests your doctor would ask you to undergo to assess your situation. The follow-up tests will look for the hCG hormone levels, and whether they have returned to normal or not. The doctor will also look for tubal or ectopic pregnancy. If the couple is facing multiple chemical pregnancies, the doctor will look for a treatable cause such as an infection or a uterine abnormality. The treatments in such cases include
- Antibiotics to fight any infections
- Surgery to correct the uterine abnormality
- Progesterone
- Baby aspirin
- Counselling
Can You Prevent a Chemical Pregnancy?
Unfortunately, there are no methods to prevent a chemical pregnancy in the general population. However, if you have a medical condition that predisposes you to one, the condition can be treated to improve your chances.
When Can You Try to Get Pregnant Again After a Chemical Pregnancy?
Ovulation and conceiving after chemical pregnancy are possible as early as two weeks after the miscarriage. But it is recommended that you wait for at least one normal menstrual cycle before trying to become pregnant again. Also, it is better to run tests to screen for any medical problems before trying again.
Tips for Getting Pregnant After a Chemical Pregnancy
While it may take time, many women go on to have successful pregnancies after a chemical pregnancy. Here are some helpful tips to increase your chances of getting pregnant again:
- Allow Time for Your Body to Recover: While it’s possible to conceive right after a chemical pregnancy, allowing your body to return to its normal cycle can help ensure a healthy pregnancy. It’s generally advised to wait at least one full cycle before trying again.
- Maintain a Healthy Lifestyle: Prioritise a balanced diet, regular exercise, and stress management. Maintaining overall health can help balance hormones and increase your chances of a successful pregnancy.
- Track Ovulation: Using ovulation tracking tools, such as temperature charting or ovulation predictor kits, can help you identify the most fertile days of your cycle, making it easier to time intercourse.
- Consult with a Healthcare Provider: If you’ve had multiple chemical pregnancies, consider speaking with a healthcare provider or fertility specialist. They can offer guidance and check for any underlying conditions that may need treatment before trying to conceive again.
Other Important Things You Should Know About a Chemical Pregnancy
- There is no evidence to suggest that a chemical pregnancy will affect future pregnancies. Many women have gone on to have healthy pregnancies after a chemical pregnancy.
- For couples who are trying through an IVF, a chemical pregnancy is also a good indicator as it is a sign of implantation and pregnancy. This shows the potential for further attempts to be successful.
FAQs
1. Does a chemical pregnancy mean there is a problem with my reproductive health?
A chemical pregnancy does not necessarily indicate a problem with your reproductive health. Often, it happens due to chromosomal abnormalities that prevent the embryo from developing properly. However, if chemical pregnancies occur frequently, it might be helpful to consult a fertility specialist to rule out underlying health conditions.
2. Can stress cause a chemical pregnancy?
While stress is often linked to various health conditions, there is limited evidence to suggest that it directly causes chemical pregnancies. However, stress can impact overall health, including hormone levels, which may play a role in early pregnancy losses.
3. Can a chemical pregnancy be triggered by medications or treatments?
Certain medications, such as those used in fertility treatments or hormonal therapies, could potentially affect pregnancy outcomes. Though rare, some women may experience a chemical pregnancy as a side effect of medications that influence hormone levels or uterine conditions, like progesterone supplements or ovulation induction drugs.
Chemical pregnancies can happen to any woman and are mostly not under their control. It is possible to have healthy pregnancies after one or more chemical pregnancies as well. If you are concerned or have questions about chemical pregnancy, reach out to a gynaecologist to understand this condition better.
References/Resources:
1. Chemical Pregnancy; Cleveland Clinic; https://my.clevelandclinic.org/health/diseases/22188-chemical-pregnancy
2. What Is a Chemical Pregnancy?; Penn Medicine Lancaster General Health; https://www.lancastergeneralhealth.org/health-hub-home/motherhood/getting-pregnant/what-is-a-chemical-pregnancy
3. FAQS: Early Pregnancy Loss; American College of Obstetricians and Gynecologists; https://www.acog.org/womens-health/faqs/early-pregnancy-loss
4. Chemical Pregnancy; American Pregnancy Association; https://americanpregnancy.org/getting-pregnant/pregnancy-loss/chemical-pregnancy/
5. Coulam. C, Roussev. R; Chemical pregnancies: immunologic and ultrasonographic studies (American Journal of Reproductive Immunology); National Library of Medicine; https://pubmed.ncbi.nlm.nih.gov/12516655/; November 2002
6. Early Pregnancy Loss; FamilyDoctor.org.; https://familydoctor.org/condition/early-pregnancy-loss/
7. Chemical pregnancy; Miscarriage Association; https://www.miscarriageassociation.org.uk/information/miscarriage/chemical-pregnancy/
Also Read:
Abdominal Pregnancy
Heterotopic Pregnancy
Types of Twin Pregnancy
Different Kinds of Pregnancy
Was This Article Helpful?
Parenting is a huge responsibility, for you as a caregiver, but also for us as a parenting content platform. We understand that and take our responsibility of creating credible content seriously. FirstCry Parenting articles are written and published only after extensive research using factually sound references to deliver quality content that is accurate, validated by experts, and completely reliable. To understand how we go about creating content that is credible, read our editorial policy here.