Cholera: Causes, Symptoms, Treatment, and Vaccination

According to WHO, approximately 1.3 to 4 million reported cases of cholera surface worldwide every year (1). Unsafe sanitary conditions and poor hygiene affect food and drinking water, making them unfit for consumption. Cholera disease is a severe bacterial illness primarily spread through contaminated water. Cholera is a common bacterial infection in regions where water and food are not handled hygienically. An acute diarrhoeal and intestinal disease, cholera can kill within hours if left untreated due to rapid dehydration. Although often called the cholera virus, it is actually caused by bacteria, not a virus. Clean drinking water and proper sanitation are essential to prevent outbreaks. To combat cholera, we first need to learn how it starts, its risks, and whether there is a vaccine for it.
What Is Cholera and How Common Is It?
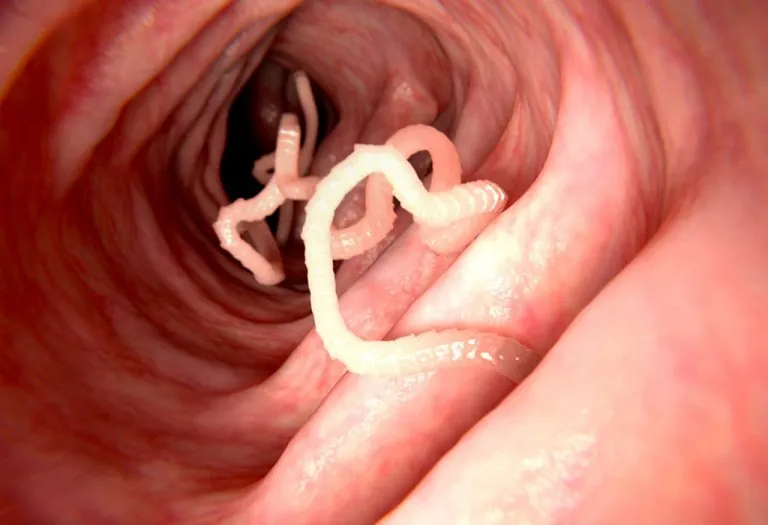
Cholera is an acute intestinal infection known to spread through unhygienic food and water contaminated with the bacterium VIbrio cholerae (1). It does not spread from person to person but can spread through contact with the faeces of the infected person. The cholera bacterium (Vibrio cholerae) attacks the intestines of the infected individual and causes vomiting, diarrhoea, and subsequent loss of fluids. In grave cases with no treatment, it can severely dehydrate the person and lead them into shock and later death.
Cholera is common in several parts of the Caribbean, Southeast Asia, South America, Africa, and the Pacific, usually where the climate is warm or where natural disasters like hurricanes or earthquakes happen (2). If people travelling to these places don’t follow hygiene practices, the infection can be risky.
Expert Says
“Improved personal hygiene, access to clean water, and sanitation are the mainstays of cholera control.”
– Dr. Vandan H Kumar
Types of Cholera
Cholera is a severe diarrheal disease caused by Vibrio cholerae, and its occurrence can be categorised into two main types. These classifications depend on the frequency and spread of the disease in a given population.
1. Endemic Cholera
Endemic cholera refers to regions where the disease is consistently present at a baseline level, often due to poor sanitation and limited access to clean water. Countries in South Asia, sub-Saharan Africa, and parts of Latin America frequently experience endemic cholera. In these areas, outbreaks may occur seasonally but remain relatively predictable.
2. Epidemic Cholera
Epidemic cholera occurs when there is a sudden, large-scale outbreak in areas where the disease is not normally present. These outbreaks often follow natural disasters (e.g., floods or earthquakes), conflicts, or humanitarian crises that disrupt water and sanitation systems. Epidemic cholera spreads rapidly and can cause high mortality if not controlled quickly.
Causes of Cholera
The disease is linked to poor sanitation conditions affecting food and water. The primary cause of cholera disease transmission is the bacterium—Vibrio cholerae, which is found in faeces. When people ingest food or water contaminated with this bacterium, they contract the disease (3).
- Poor Sanitation:- Peri-urban slums, refugee camps, and poor colonies, where proper facilities for clean water and sanitation are not available are high-risk areas.
- Water:- People living in crowded conditions and sourcing water from common water sources have chances of getting cholera. Public wells with the possibility of contamination is a common example.
- Raw Fruits and Vegetables:- In developing countries where cholera is common, irrigation water or uncomposted manure fertilizersfertilisers mixed with raw sewage can contaminate the fields. Hence, the raw produce, including fruits and vegetables, can be a source of cholera.
- Seafood:- Seafood, mostly shellfish, contains cholera and hepatitis A virus that come from places bearing cholera. In search of food, shellfish filter litres of water and thus catch cholera bacteria and other viruses from water.
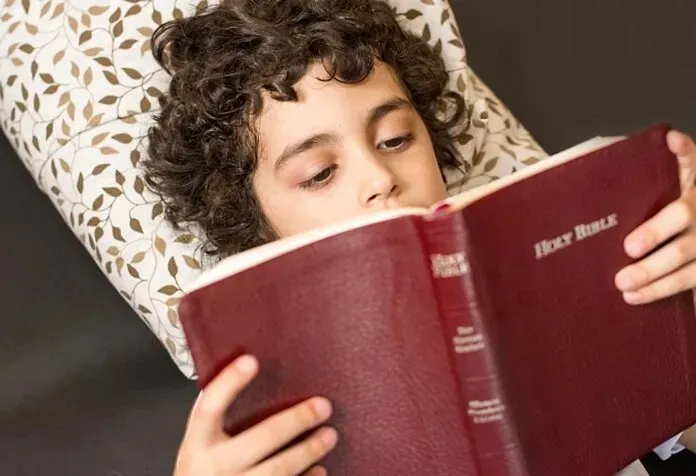
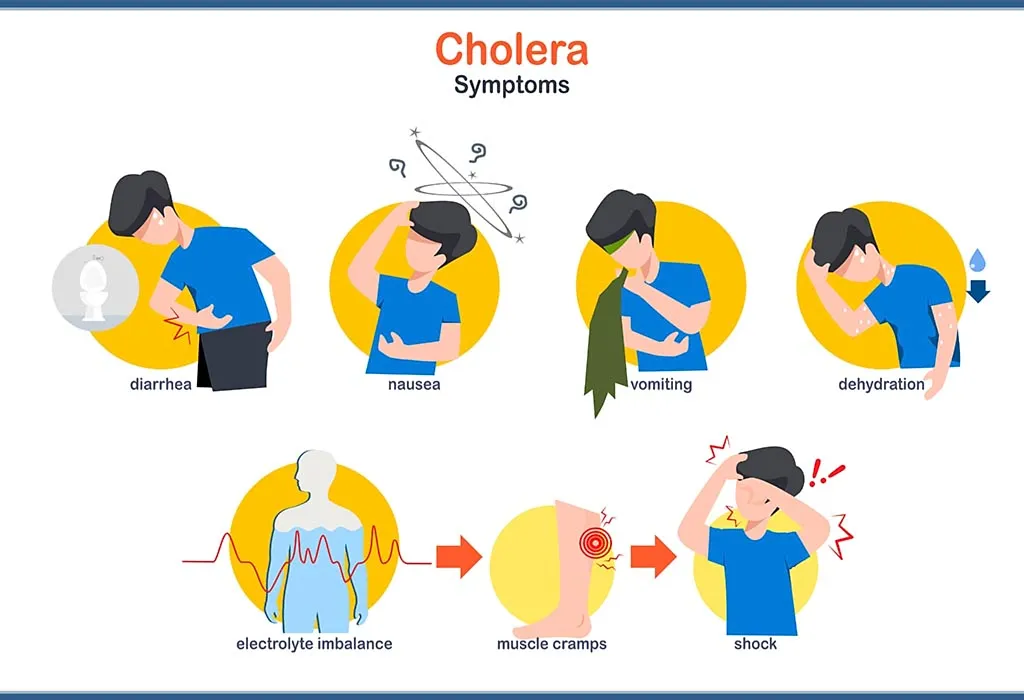
Symptoms of Cholera
The cholera bacteria symptoms generally surface between 12 hours and five days of ingestion of contaminated food and water (4). Some of the commonly observed signs and symptoms of cholera, according to Mayo Clinic are (5):
- Profuse watery diarrhoea
- Dehydration
- Vomiting
- Rapid Fluid Loss
- Leg Cramps
- Shock
The symptoms of cholera typically range from mild to moderate, with cases of mild dehydration and diarrhoea. However, even mild symptoms can make the person weak and irritated. In severe cases, vomiting and diarrhoea cause the person to lose body fluids faster than usual.
If left untreated, cholera can lead to shock and death within hours. Cholera can lead to premature delivery or miscarriage in pregnant women (6).
What Are the Risks and Complications of Cholera?
Cholera can be a result of a humanitarian crisis and can affect anyone working in those conditions. However, infants have fewer chances of developing this illness as they get immunity from their mother’s breast milk, who previously had cholera. Still, there linger risk factors that can make anyone susceptible to this infection.
Risks
Cholera poses serious health risks, particularly in areas with poor sanitation and limited clean water access. The disease can lead to severe dehydration, organ failure, and even death within hours if left untreated, making rapid intervention critical.
- Poor Sanitation: Poor sanitary conditions harbour many bacteria and viruses, causing illnesses like cholera. Developing countries, refugee camps, and places where hygiene is still in a developing phase are most affected.
- Close Exposure: If you are living with someone who has cholera, the chances of contracting this illness increases twofold.
- Low Stomach Acid: The stomach acid acts as a defence system against cholera bacteria. However, people with low stomach acid content, including children, older adults, and people who usually take antacids, proton pump inhibitors, or H-2 blockers to reduce the stomach acid, are at a high risk of cholera.
- Shellfish: Eating raw or undercooked shellfish from the waters of cholera-bearing places can put you at risk of developing this disease.
- Type O Blood: Although the reason isn’t quite clear, people with type O blood are more likely to develop cholera than other blood types.
Complications
Cholera can be easily treated. With timely treatment, the fatality of the infection can be reduced to just 1%.
- Loss of Electrolytes and Low Blood Sugar (Hypoglycaemia): Low blood sugar (glucose) due to diarrhoea and poor appetite can cause severe complications. This can result in unconsciousness, seizures, or even death.
- Kidney Failure: In severe cases, cholera can cause kidney failure and cause body fluids and waste to build in the body, creating life-threatening scenarios.
- Low Potassium: Rapid fluid loss and electrolytes from cholera can deplete potassium levels, potentially affecting heart and nerve functions and becoming life-threatening.
How Is Cholera Diagnosed?
Cholera is diagnosed through a combination of clinical evaluation and laboratory testing, as its symptoms can resemble other diarrheal illnesses. Here are the diagnostic methods for cholera:
- Clinical Assessment: Doctors evaluate symptoms like severe watery diarrhoea, vomiting, and rapid dehydration.
- Stool Culture: The gold standard—stool samples are tested for Vibrio cholerae in a lab.
- Rapid Diagnostic Tests (RDTs): Dipstick tests provide quick results in resource-limited settings.
- Microscopy (Dark-Field Examination): Reveals the darting motility of Vibrio cholerae under a microscope.
- PCR (Polymerase Chain Reaction): Detects cholera DNA for highly accurate confirmation.
- Serotyping: Identifies whether the strain is O1 or O139, the main epidemic-causing serogroups.
- Antibiotic Sensitivity Testing: Determines effective treatments if drug resistance is suspected.
- Environmental Testing: Checks water sources for contamination during outbreaks.
How Is Cholera Treated?
Cholera can be easily treated. With timely cholera treatment, the fatality of the infection can be reduced to just 1%.
- Rehydration: The majority of cases can be treated through oral rehydration. In the oral rehydration method, oral rehydration salt (ORS) powder is taken by diluting it with water to control dehydration. It is essential for patients to drink plenty of fluids to avoid dehydration.
- Intravenous Fluids: In case of severe dehydration, patients are at risk of shock and may require the administration of intravenous fluids.
- Antibiotics: Antibiotics also help reduce the duration of the severity of the infection. However, this treatment is less critical than rehydration.
- Zinc Supplements: Zinc supplements are effective in treating children under five years. Zinc reduces diarrhoea and shortens the episodes of acute cholera.
- Breastfeeding: Breastfeeding is also encouraged to treat this illness.
How Can Cholera Be Prevented?
If you are residing in a region affected with cholera sickness or travelling to places with cholera outbreaks, these methods will help prevent you from developing cholera (7):
- Practice hand hygiene: Washing hands with soap and water thoroughly before handling the food and after using the toilet is necessary. Rub your soapy hands for at least 15 to 20 seconds to remove the germs and grime. Alternative to soap and water is alcohol-based hand sanitiser.
- Drink clean water: Drink only boiled or purified water. Bottled water is also good. If you are going out, drinking hot or bottled beverages is safe. Also, use ice that is made using boiled and purified water only.
- Eat hot and properly cooked food: To avoid cholera, it’s best to eat hot and properly cooked food. Avoid food from street vendors as much as possible. Packaged food is preferable.
- Eat fruits that can be peeled: Fruits and vegetables in cholera-affected places may carry cholera bacteria on their peels. Hence, avoid fruits that can’t be peeled. For example, consume oranges and bananas and avoid fruits like grapes and berries.
- Avoid raw fish: If you are likely to be affected by cholera, avoid raw or undercooked seafood, such as sushi and shellfish.
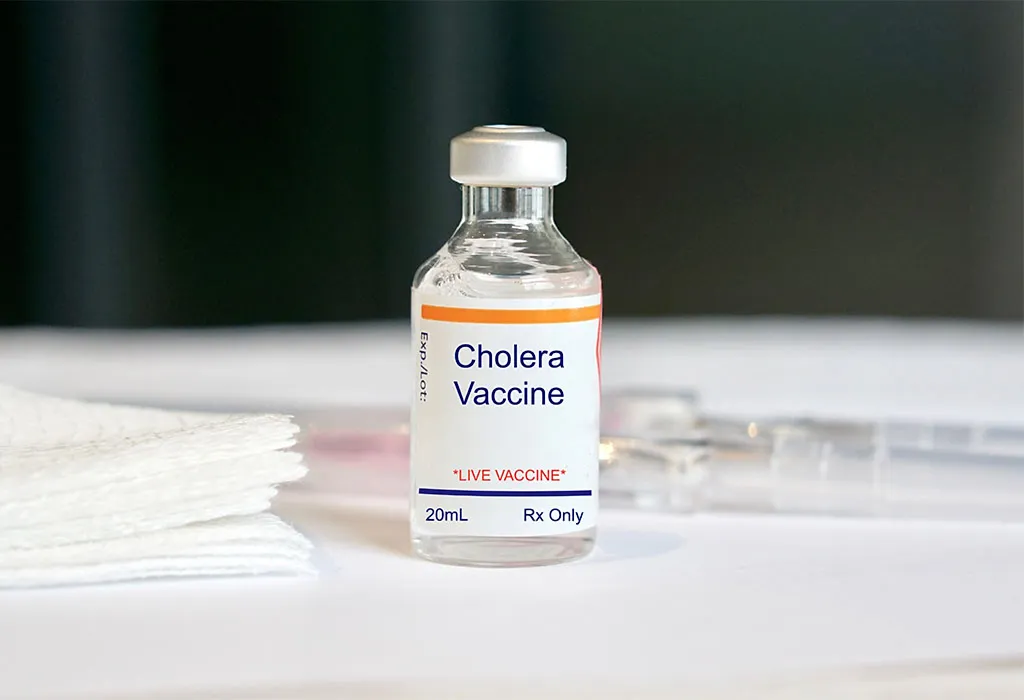
- Vaccination: Cholera vaccine is also beneficial in preventing illness.
What Is Cholera Vaccine and How Does it Work?
The cholera vaccine is a prescription vaccine used to fight against cholera bacteria. The vaccine is an inactivated vaccine made using dead cholera-causing bacteria. The vaccine instructs the host body to produce antibodies to protect against cholera bacteria. The vaccine is given orally (via mouth) to the individual. The Oral Cholera Vaccine (OCV) is a two-dose vaccine administered at an interval of at least two weeks. It is available in powder form, which is mixed with water for consumption. The vaccine is available at healthcare centres across India.
Why Should You Get Vaccinated?
Anyone can develop this illness because of unsafe drinking and eating conditions. Vaccination is one of the best lines of defence against the bacteria causing cholera. Oral Cholera Vaccine (OCV) is taken orally. Hence, it is painless and more effective.
The vaccine is highly recommended for individuals travelling to places with active cholera infections or where the disease is common.
When Should You Take the Cholera Vaccine?
Anyone above the age of one can take the cholera vaccine orally. You must notify your doctor before receiving the vaccine if you have ever had an adverse response to a vaccine. Because some medications may interact with the cholera vaccination, it is wise to tell your doctor what medications you are currently taking.
The vaccine is to be taken on an empty stomach, at least 1 hour before or 1 hour after eating. The individual must refrain from drinking, eating, or taking any other drug by mouth for an hour before and after taking the cholera vaccine.
What Are the Side Effects of the Cholera Vaccine?
The commonly observed side effects of the cholera vaccine are (8):
- Fever
- Vomiting
- Nausea
- Abdominal pain
- Cough
- Weakness
- Rash
- Itching
- Dryness in mouth
Most of these side effects are common and disappear on their own. If they still persist, consult your doctor.
Can You Take the Cholera Vaccine During Pregnancy?
Because of the limited evidence of the efficacy of the non-live vaccine, including the oral cholera vaccine, in pregnant women, it is best to consult the doctor before taking the cholera vaccine in pregnancy (9) (10).
Is It Safe to Take the Cholera Vaccine While Breastfeeding?
The cholera vaccine is safe to use during breastfeeding (11) (12). Studies have shown that the vaccine does not pass into the breastmilk, making it safe for the baby.
Which Cholera Vaccine Is Available in India?
Currently, the oral cholera vaccine available to use in India is Shanchol™. Shanchol™ is a WHO-prequalified oral cholera vaccine (OCV) licensed for use in India. It is manufactured by Shantha Biotech (a Sanofi Company) in Hyderabad. Shanchol™ is a bivalent (BivWC)/whole killed cell (only) vaccine as it incorporates newly emerged O1 and O139 serogroups of V. cholerae (13).
The vaccine is administered with a gap of 2 weeks between doses and provides protection for at least three years. It can be given to all individuals over the age of one. Shanchol™ was licensed in India in 2009 and obtained WHO prequalification in 2011.
When to Call the Doctor?
Cholera is usually found in places where hygiene and sanitation are not maintained. If you have developed severe dehydration and diarrhoea after visiting such a place or eating anything unhygienic, it’s best to seek medical consultation immediately from a doctor.
FAQs
1. What should you do if you miss a dose of the vaccine?
If you miss out on the dose of cholera vaccination during the stipulated time, you can consult with your doctor for a catch-up vaccine.
2. Which things should I avoid after receiving the vaccine?
You must avoid drinking, eating, and taking any medicines for at least one hour after taking the vaccine, as it may reduce the vaccine’s efficacy.
3. Are there any drugs that affect the cholera vaccine?
Some medications may react to the cholera vaccine. Hence, it is best to consult your doctor and inform them about the medications you are taking.
Cholera can be a cause of the humanitarian crisis but can be easily treated and prevented using a multifaceted approach. Frequent checks on sanitation and hygiene, surveillance, and mobility of oral cholera vaccines can limit cholera from multiplying in society. Maintaining good personal hygiene and being careful about what you eat and drink is essential to prevent foodborne and waterborne diseases like cholera. Talk to your doctor about cholera vaccination.
References/Resources:
4. European Centre for Disease Prevention and Control – Cholera
6. National Library of Medicine – Cholera Infection Risks and Cholera Vaccine Safety in Pregnancy
7. Journal of Clinical and Diagnostic Research – Why is the Oral Cholera Vaccine Underused in India?
8. CDC – Vaccine Information Statements (VIS)
10. JAMA Network – Cholera Vaccine Safe During Pregnancy
11. Specialist Pharmacy Service NHS – Using vaccines during breastfeeding
12. National Institute of Child Health and Human Development – Cholera Vaccine
Also Read:
Pneumococcal Vaccine
Meningococcal Vaccination
Childhood Vaccinations for Various Diseases
Here’s What You Need to Know About Meningitis
Common Monsoon Diseases in Babies and Children
Was This Article Helpful?
Parenting is a huge responsibility, for you as a caregiver, but also for us as a parenting content platform. We understand that and take our responsibility of creating credible content seriously. FirstCry Parenting articles are written and published only after extensive research using factually sound references to deliver quality content that is accurate, validated by experts, and completely reliable. To understand how we go about creating content that is credible, read our editorial policy here.














.svg)