Jaundice in Pregnancy: Causes, Symptoms, & Treatments

- Causes of Jaundice in Pregnancy
- Signs and Symptoms of Jaundice When Pregnant
- Diagnosing Jaundice During Pregnancy
- Risks and Complications of Jaundice During Pregnancy
- Treatments for Jaundice During Pregnancy
- Diet Plan for Jaundice in Pregnant Women
- How to Prevent Jaundice While Pregnant?
- Natural Home Remedies for Pregnancy Jaundice
- When Should You Consult the Doctor?
- FAQs
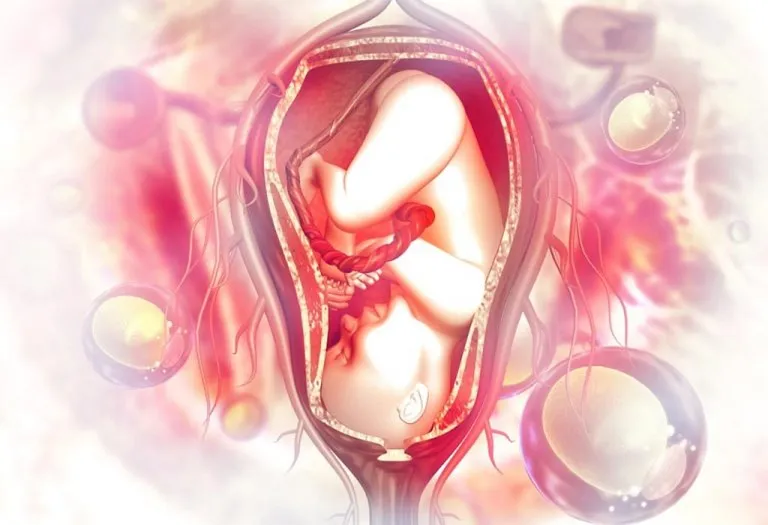
Jaundice is caused when the liver does not function properly, leading to the accumulation of bilirubin in the body. The most visible symptom of jaundice is the yellowish discolouration of the sclera of the eyes, skin, and urine. Jaundice in pregnancy can be particularly concerning as it may indicate underlying liver issues. Liver disease during pregnancy includes a spectrum of diseases that may occur during pregnancy and the postpartum period, resulting in abnormal liver function tests, hepatic and biliary system dysfunction, or sometimes both.
Jaundice and pregnancy together can present unique challenges for diagnosis and management, requiring careful monitoring. It is observed in 3 to 10% of all pregnancies, necessitating awareness and timely intervention to ensure the health and safety of both the mother and the developing fetus.
Causes of Jaundice in Pregnancy
Jaundice in pregnancy can arise from various medical conditions that affect liver function or bile flow during this delicate period. Below are some of the common causes that can lead to jaundice during pregnancy (1).
Pregnancy-specific Causes
- Hyperemesis Gravidarum – A condition where the mother-to-be experiences severe nausea accompanied by vomiting, electrolyte imbalance and weight loss (2).
- Intrahepatic Cholestasis – A condition characterised by severe itching, as the normal flow of bile is interrupted (3).
- Pre-eclampsia – A condition where the mother has very high blood pressure, and there is protein in the urine (4).
- HELLP Syndrome – This is a liver disorder which is believed to be a severe form of pre-eclampsia and may be life-threatening (5).
- Acute Fatty Liver – A liver disorder characterised by the accumulation of excessive fat in the liver (6).
Causes Unrelated to Pregnancy
- Primary Liver Disorders:
- Acute Viral Hepatitis: HAV(Hepatitis A Virus) / HEV(Hepatitis E Virus)
- Drug-induced hepatitis: PCM (paracetamol) overdose
- Chronic hepatitis HBV (Hepatitis B Virus) / HCV(Hepatitis C Virus)
- Autoimmune hepatitis
- Wilson’s disease
- Cirrhosis of Liver
- Budd Chiari syndrome
- Pre-Hepatic (Liver) Causes: Conditions causing hemolytic anaemia like Malaria and Sickle Cell Anaemia.
- Secondary Causes: Obesity, certain autoimmune diseases, congenital malformation or raised cholesterol levels.
Signs and Symptoms of Jaundice When Pregnant
Following are the common signs & symptoms of jaundice in pregnancy (7):
- Yellowing of the eyes
- Yellowish tinge to the skin
- Dark coloured urine
- Itching
- Light coloured stools
- Weakness
- Loss of appetite
- Headache
- Nausea and vomiting
- Fever
- Swelling around the liver region
- Swelling of the legs, ankles, and feet
Diagnosing Jaundice During Pregnancy
Diagnosing liver disease during pregnancy can be challenging and depends on laboratory investigations. Signs and symptoms are mostly not very specific and can include vomiting and pain in the stomach. The causative disease of jaundice can have a significant effect on the outcomes in both the mother and the baby and requires a battery of tests to be run. Here are the main ways in which jaundice is diagnosed:
1. Clinical Evaluation
Here it may show skin changes, such as redness of palms of hands and cherry-like skin lesions. These changes occur due to high levels of oestrogen in pregnant women and occur in about 60% of healthy pregnancies.
2. Abnormalities in Laboratory Test Results
Lab tests that show a low level of albumin (a plasma protein) in serum elevated ALP or alkaline phosphatase, and elevated prothrombin time (PT) indicate a problem.
3. Diagnostic Imaging
Ultrasonography is the first choice since it is free of radiation risk to the foetus. Magnetic resonance imaging (MRI) may also be used. It is relatively safer than computed tomography (CT) and endoscopic retrograde cholangiopancreatography (ERCP), which are more specific diagnostic tools but involve a risk of radiation hazard for the baby.
Risks and Complications of Jaundice During Pregnancy
The effects on the foetus because of jaundice in pregnancy are many. Risks include maternal and delivery-related problems as well as the direct impact on the foetus.
Maternal health risks include fulminant (severe impairment of liver function) or severe hepatitis (if not treated), hepatic encephalopathy (a neurological complication of severe liver damage), liver damage-induced kidney problems like hepatorenal syndrome, liver Cirrhosis, abnormal bleedings like haemorrhagic varies, and risk of liver malignancy in a few cases.
Delivery-related complications include preterm deliveries, stillbirths, abruption placenta and postpartum haemorrhages, and risk of transmission of infections in the newborn during delivery.
Risks to the newborn include IUGR (intrauterine growth restriction), congenital hepatitis and neurological complications including kernicterus (brain damage in a newborn due to jaundice) and cerebral palsy in severe cases.
Treatments for Jaundice During Pregnancy
Treatment of jaundice during pregnancy is based on the causative factor and is majorly dependent on the time of recognition of the symptoms and the stage of pregnancy.
Common lines of treatment, irrespective of the cause of jaundice, include,
- Dietary Measures: Diets low in proteins and avoiding food and drugs harmful to the liver
- General Supportive Measures: Adequate rest, hydration, continuous monitoring of vital parameters like BP and urine output, supplemental oxygen and blood components as and when required with an intensive care facility
Specific management of jaundice depends upon the underlying conditions:
- Antivirals, vaccinations and interferons in viral hepatitis
- Antithrombotics in Budd Chiari syndrome or EHVT
- Treatment of specific causes of any hemolytic anaemia
- Surgical banding for variceal haemorrhages
- Shunt surgeries in cirrhosis of the liver
- Liver transplantation in end-stage liver disease
Diet Plan for Jaundice in Pregnant Women
Managing jaundice during pregnancy requires special attention to diet to support liver function and overall health. Here are the foods to eat and foods to avoid when you have high bilirubin during pregnancy (8).
Foods to Eat
Choosing the right food for jaundice in pregnancy is essential to support liver health and recovery. A nutritious diet can help manage symptoms and ensure the well-being of both mother and baby.
- Fruits like apples, pears, oranges, spinach, and kale are rich in antioxidants and essential nutrients that support liver health.
- Lean Proteins like skinless chicken breast, salmon, and tofu provide high-quality protein without excessive fat, aiding in liver recovery.
- Whole Grains like brown rice, quinoa, and oats offer fibre and essential nutrients that support digestive health and detoxification.
- Drinking plenty of water and herbal teas like peppermint and chamomile helps you stay hydrated and aids in flushing out toxins.
Foods to Avoid
Knowing which food causes jaundice during pregnancy can help in making better dietary choices that support liver function and overall well-being.
- Items like French fries, fried chicken, and pastries can increase liver strain and contribute to inflammation.
- Foods high in added sugars, salt, and artificial additives, such as canned soups and sugary snacks, can burden the liver.
- Any form of alcohol can severely impact liver function and should be avoided during pregnancy.
- Whole milk, cheese, and creamy sauces can be high in saturated fats, which may stress the liver.
- Fatty cuts of beef and pork can be harder for the liver to process and should be limited.
How to Prevent Jaundice While Pregnant?
Preventing jaundice during pregnancy involves taking the following proactive steps to support liver health and reduce the risk of complications.
1. Healthy Diet
You must consume fatty products like dairy foods and meat only in the recommended quantities, as excessive consumption may further affect your liver.

2. Healthy Weight
Maintain a healthy weight and regulate cholesterol levels in the blood
3. Regular Immunisations
Hepatitis can be prevented with effective vaccination. Your gynaecologist will advise you about it
4. Limit the Consumption of Drugs
Avoid taking drugs or compounds that can be toxic to the liver. You should ask your doctor before popping any pills during pregnancy, as these can be harmful to your baby
5. Be Alert While Travelling
Avoid travelling to regions that have a breakout of diseases like malaria. The malarial parasite destroys red blood cells, and this may lead to jaundice.
6. Measuring and Reducing Risk Factors
Go for regular checkups. Seek medical help as soon as you notice symptoms of jaundice to avail early treatment and to ensure a speedy recovery. Jaundice during pregnancy can be managed when diagnosed in time.
Natural Home Remedies for Pregnancy Jaundice
You may also consider some home remedies for the treatment of jaundice during pregnancy. These are not medically proven, but you can try them in addition to your treatment for a faster recovery.
- Drinking fenugreek tea two to three times a day is very helpful in curing jaundice.
- Drinking one glass of tomato juice with a pinch of salt and pepper taken on an empty stomach in the morning is quite effective for jaundice.
When Should You Consult the Doctor?
It’s important to consult a doctor if you experience symptoms of jaundice during pregnancy to ensure proper diagnosis and treatment. Timely medical intervention can help manage the condition effectively and safeguard both maternal and fetal health.
- Persistent Yellowing: If you notice persistent yellowing of the skin or eyes that does not improve, seek medical advice.
- Severe Abdominal Pain: Consult your doctor if you experience significant or worsening abdominal pain, which may indicate liver complications.
- Unexplained Fatigue: If you have extreme fatigue or weakness that is not explained by other factors, it’s important to get a medical evaluation.
- Dark Urine or Pale Stools: Changes in urine color to dark brown or stool color to pale can signal liver dysfunction and warrant a doctor’s visit.
- Nausea and Vomiting: Persistent nausea or vomiting, especially if accompanied by jaundice symptoms, should be evaluated by a healthcare professional.
FAQs
1. Can jaundice in pregnancy affect the baby’s development?
While jaundice in pregnancy mainly affects the mother, it can sometimes lead to complications that impact the baby, making it important to monitor and manage the condition closely.
2. Can stress exacerbate jaundice symptoms during pregnancy?
Chronic stress can impact liver function and potentially worsen jaundice symptoms, making stress management an important part of overall treatment and recovery.
3. What are the long-term effects of jaundice in pregnancy on liver health?
If not managed properly, jaundice in pregnancy can lead to long-term liver issues, so it’s crucial to follow medical advice and monitor liver function even after symptoms improve.
4. Is there a difference in treatment for jaundice caused by viral infections versus other conditions during pregnancy?
Yes, the treatment for jaundice can vary depending on the underlying cause, such as viral infections or other liver conditions, so a precise diagnosis is essential for appropriate management.
5. Can jaundice in pregnancy lead to complications with anaesthesia during delivery?
Jaundice can sometimes impact liver function, which might complicate anaesthesia administration during delivery, so it’s important to discuss this with your healthcare provider beforehand.
6. How does jaundice during pregnancy affect breastfeeding?
Jaundice itself may not directly impact breastfeeding, but underlying liver issues could affect milk production or quality, so monitoring and consultation with a lactation specialist may be necessary.
7. Can jaundice during pregnancy recur in future pregnancies?
Yes, some conditions like intrahepatic cholestasis of pregnancy (ICP) have a high chance of recurring in future pregnancies. Women who experienced jaundice in one pregnancy should inform their doctor early in subsequent pregnancies.
Liver disease during pregnancy could be a mild disease with very few symptoms, even if you have an abnormal liver function report. The issue may be resolved on its own, or it may develop into a potentially serious condition affecting your liver. It may even lead to permanent liver damage. Viral hepatitis infection is the most common reason for pregnancy jaundice. It is usually mild to moderate disease. Active treatment may not be needed except in hepatitis E and HSV infections.
Early detection of liver diseases in pregnancy, and an integrated approach by the treating gynaecologist, gastro physician, hepatologist and transplant specialist can help you manage the condition safely.
References/Resources:
2. Cleveland Clinic – Hyperemesis Gravidarum
3. National Library of Medicine – Pregnancy Intrahepatic Cholestasis
5. Cleveland Clinic – HELLP Syndrome
6. Cleveland Clinic – Acute Fatty Liver of Pregnancy
7. Cleveland Clinic – Adult Jaundice
Also read:
Listeria when Pregnant
Chickenpox while Pregnant
Typhoid during Pregnancy
Toxoplasmosis in Pregnancy
Was This Article Helpful?
Parenting is a huge responsibility, for you as a caregiver, but also for us as a parenting content platform. We understand that and take our responsibility of creating credible content seriously. FirstCry Parenting articles are written and published only after extensive research using factually sound references to deliver quality content that is accurate, validated by experts, and completely reliable. To understand how we go about creating content that is credible, read our editorial policy here.