Mastitis – Signs, Symptoms and Treatment

Breastfeeding is highly encouraged for several important reasons beyond just providing nutrition and immunity; the baby also forms a strong emotional bond with the mother through this intimate process. However, breastfeeding can sometimes be hampered if the mother develops a painful infection called mastitis. This condition affects nursing by causing inflammation, discomfort, and, at times, forcing the mother to stop breastfeeding altogether. Understanding mastitis is crucial for new mothers to manage and prevent it effectively. Let us explore this condition in depth by examining its causes, symptoms, and treatment options in detail to ensure a smoother breastfeeding journey.
What Is Mastitis?
Here’s the mastitis meaning. Mastitis in the breast is basically a swelling or lump in the breast accompanied by pain, tenderness and redness (1). Mothers commonly experience the condition of acute mastitis within three months of their delivery. It is not restricted to breastfeeding mothers but can affect women in general. Women who have any kind of chronic health problem, or a lifestyle disease like diabetes, are also likely to suffer from mastitis (whether they be new mothers or not). Cancer too, can lead to mastitis.
How Common Mastitis Is?
Mastitis is a fairly common condition, particularly among breastfeeding mothers. Studies suggest that up to 3–20% of lactating women may experience mastitis at some point, most often within the first three months postpartum (2). However, it can occur at any stage during breastfeeding.
Types of Mastitis
Mastitis, an inflammation of breast tissue, can arise from various causes and manifest in different forms. Recognising these different types is crucial for effective diagnosis and management. Here are three common types of mastitis (3):
1. Lactational Mastitis
Lactating mastitis is the most common type and typically affects breastfeeding women. It usually occurs within the first few weeks or months postpartum. This type of mastitis often results from milk stasis (when milk isn’t effectively removed from the breast), a blocked milk duct, or bacteria entering the breast through a cracked nipple. Symptoms can include breast pain, redness, warmth, swelling, and flu-like symptoms such as fever and chills.
2. Idiopathic Granulomatous Mastitis (IGM)
Idiopathic granulomatous mastitis (IGM) is a rare, benign, chronic inflammatory condition of the breast. The term “idiopathic” means the cause is unknown, and “granulomatous” refers to the specific pattern of inflammation seen under a microscope. IGM typically affects women of childbearing age, even those who are not currently breastfeeding. Symptoms can include firm, often painful lumps in the breast, skin redness, swelling, and sometimes skin ulceration or nipple retraction. The course of IGM is variable, and treatment can range from observation to medications or surgery.
3. Periductal Mastitis
Periductal mastitis is a specific type of non-lactational mastitis that primarily affects the area around the milk ducts near the nipple. It is often associated with smoking. Inflammation and blockage of the milk ducts are characteristic features. Symptoms can include nipple pain, a tender lump beneath the areola, nipple retraction, and sometimes a thick, discoloured nipple discharge. Recurrent infections and the formation of abscesses are also possible with this type of mastitis.
Causes of Mastitis
As explained previously, mastitis refers to swelling, enlargement, or inflammation of breasts. There are several causes for mastitis.
In new mothers, breast inflammation is most commonly caused as a result of infection by bacteria coming from the baby’s mouth, that enter the milk ducts of the breast through fine cracks in the nipples during breastfeeding. While this is not common, between 1 and 3 percent of new mothers suffer from mastitis.
Sometimes mastitis is also caused as a result of clogged milk ducts due to insufficient breastfeeding. A baby, for various reasons, may not be able to empty the mother’s breast in one feed. At such times, milk gets accumulated in the breasts, leading to mastitis. This problem can be mitigated by regularly breastfeeding the baby. However, clogged milk ducts increase chances of mastitis caused by breast infection, and can also worsen an existing infection (4).
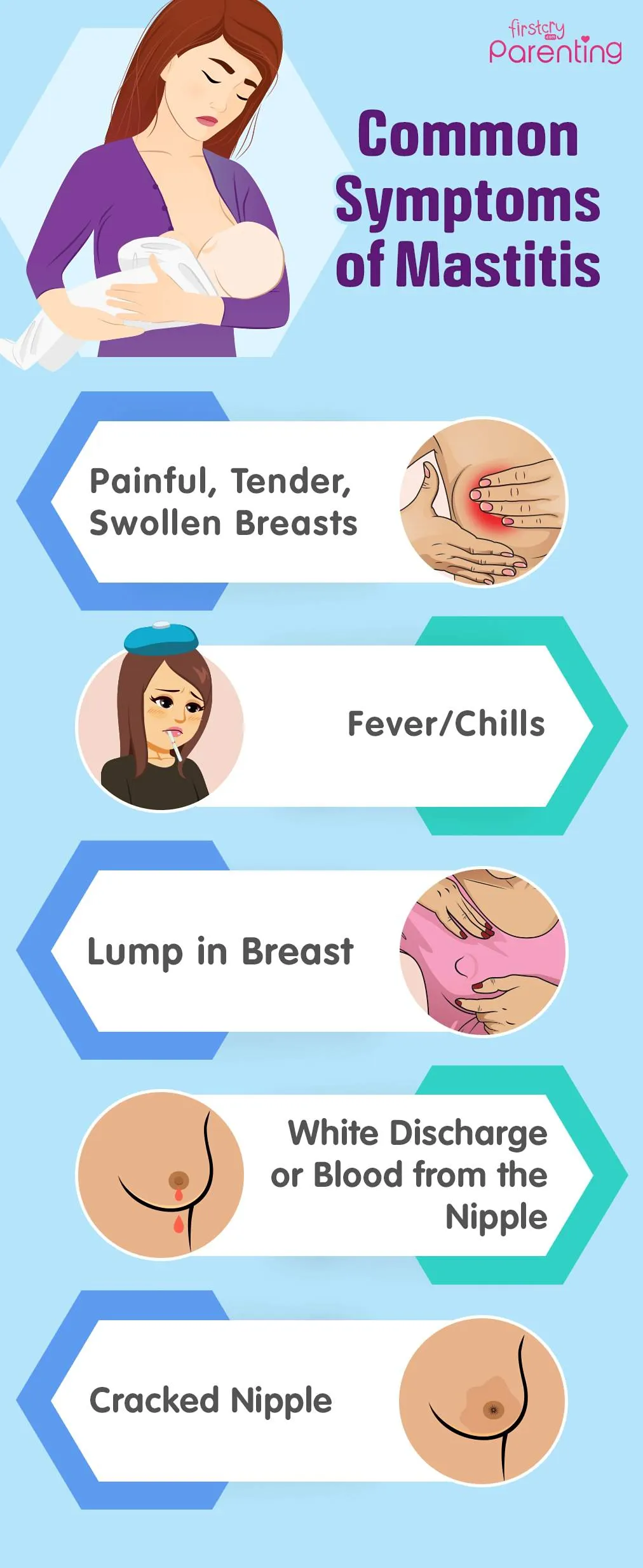
Signs and Symptoms of Mastitis
Clogged breast duct symptoms are mentioned below (5):
- You may feel that the entire breast or a part of it is painful, tender, swollen, and at times, warm. Some mothers can experience inflammation in a specific area, while others may feel the whole breast is tender.
- The most prominent sign is the formation of a hard lump on the section of breast pointing towards the nipple, which often feels tender when touched.
- Lump in the breast may leave you tired and achy. Sometimes the body shows symptoms comparable to flu, mainly chills and/or fever. If a breastfeeding mother has flu symptoms, then she is probably suffering from mastitis without feeling any other symptoms.
- You may also notice white discharge or streaks of blood from the nipple.
- A constant high fever that does not recede easily, and prolonged breast tenderness. You feel out of energy if an infection accompanies mastitis.
- Cracked nipples that bleed are a common symptom, too. You might even miss out on feedings or take longer breaks between each feed.
Non-lactational mastitis symptoms are identical to those of mastitis observed in new mothers. However, non-lactational mastitis is not as common.
Diagnosis of Mastitis (Breast Infection)
If you notice the symptoms above, then consult a doctor. Timely treatment can help reduce discomfort, prevent frequent disruption to breastfeeding and avoid other complications. You can also take lactation consultation for further assistance.
Mastitis is normally diagnosed based on the symptoms, history and medical tests. The doctor may suggest breast milk sample for culture to determine the germs affecting the condition. Based on the diagnosis, the doctor can find the underlying reason for breast soreness. Other issues can be ignored, like abnormalities in the baby’s mouth, fissures in nipples, blocked milk ducts or infection from yeast. You may be suggested to take a mammogram to diagnose a possible inflammatory form of breast cancer. It is a quite rare form of cancer that also shows symptoms similar to mastitis.
Risk Factors for Developing Mastitis
The risk factors associated with the formation of mastitis include:
- Cracked nipples that are sore are prone to infection.
- Not using the breasts equally while breastfeeding and not completely draining the milk, which can clog the ducts.
- Poor latching at the breast. If the baby fails to latch on properly, he will not suck milk properly from the breast. In fact, if you don’t nurse the baby in the correct position, it will irritate your nipples, thus increasing the risk.
- Irregular expressing or feeding.
- A tightly fitted bra.
- Multiple births.
- Family history or previous experience of mastitis.
- Poor nutrition, which could make it easier for bacteria to thrive in the mammary gland.
Complications of Mastitis
If the condition isn’t treated, it may lead to a collection of deep tissue consisting of puss or abscess in your breast, which further becomes firm due to thickening. Such a formation will need a surgical procedure to drain the abscess.
How Long Does Mastitis Last?
If diagnosed in time, mastitis can be easily treated, and recovery from it doesn’t take time. If you are suggested antibiotics then ensure you complete the course. If you notice that your breasts are still tender and you are still running a high temperature, then do reach out to your doctor.
What Should You Do If You Are Breastfeeding and Have Mastitis?
If you are a new mother, it’s crucial that you continue to breastfeed even if you have mastitis, so that the milk doesn’t accumulate. Here are some tips that can be followed:
- It may hurt while feeding but continue with the process because it will ease your problem.
- Try massaging your breast along the blocked area, starting closer to your chest, and move towards the nipple.
- Keeping warm flannels on the breasts for some time before feeding can give you some relief. This will cause let-down reflex and make the feeding process much easier for you.
- Sometimes, your baby may not be able to empty your entire breast owing to different reasons. If this is happening on a regular basis, get into the habit of pumping your milk in a bottle and then feed it to your baby.
- Change positions while feeding to help move the blockage and find the positions more effective for feeding.
Treatment of Mastitis
When it comes to mastitis therapy, normally, blocked milk duct treatment includes oral antibiotics to kill the bacteria causing infection. Another treatment is to drain out milk either through breastfeeding or pumping. This prevents more bacteria from accumulating in the breast, thus reducing the period of the infection (6).
Does Mastitis Affect Your Baby?
Even while you grapple with mastitis, know that it won’t impact your baby. They can always keep taking feeds, even from affected breasts; milk, however, may taste saltier than normal for a while. Even if the baby happens to consume the bacteria from the infection through the milk, it will be destroyed by the baby’s digestive acids. It is important to mention that the effect of mastitis antibiotics on the baby is nil. The only indirect effect that the medication has is that your milk supply could be reduced from the impacted breast.
Natural Ways to Cure Mastitis
There are some natural remedies for mastitis which you could try at home to get relief from the condition:
- You can try using a cold pack on the breast each time before you feed. Ensure it is not applied directly as it could damage the skin, and always cover it with a clean cloth before applying. The cold compress helps with the swelling condition and provides relief. Hot compress, on the other hand, can aid the clearing of the blocked ducts, and also bring about the circulation of blood and improvement in the milk flow. It can kindle your let-down reflex, which makes the process of nursing smoother.
- For mastitis treatment at home, cabbage leaves can be used as the sulphur component in them can help reduce inflammation. This could give a lot of relief to nursing mothers from issues like engorgement and blocked ducts. For this, keep a few cabbage leaves in the refrigerator for at least half an hour and then cover up your infected breast. Replace with a fresh one after the leaves placed have turned warm.
- You can try another remedy that is easily available in the kitchen. Garlic has antibiotic properties which help in killing the bacteria. Consume two raw garlic cloves in the morning as you wake up. You can also consume it with juice or water.
- Even Echinacea, a herb that strengthens the immune system could help in fighting infections. The flavonoids in the herb are known for antibiotic and antimicrobial benefits. You can also smear the solution of the Echinacea root on the affected region at least four or five times a day. Remember to clean the area properly with warm water before offering the feed.
- One of the natural cures for mastitis is apple cider vinegar with antibacterial and anti-inflammatory properties. It can help reduce swelling, combat infection and stop it from spreading. It also offers an added energy boost. For this, take one portion of apple cider vinegar and two portions of lukewarm water to make a solution and put in on the infected area. Let it stay for at least 15 minutes before washing it off. Keep repeating this twice or thrice until the infection goes away.
How to Prevent Mastitis?
To prevent mastitis, try not to wear tight-fitting tops and bras that bind your breasts tightly. Make sure you sleep on your sides as the milk tends to back up in the breasts if you end up sleeping on your back.
Ensure that your feeds are consistent and the baby is not missing out on them because it can cause breasts to engorge, leading to clogged ducts. Compressing or massaging your breast before the baby latches on is an effective method to prevent clogged ducts. You can also use a pillow designed for breastfeeding to ensure the right feeding position.
When to Consult the Doctor
Here are situations when you should consult a doctor if you have mastitis:
- Your symptoms don’t improve within 12 to 24 hours of trying home care measures.
- You develop a fever of 100.4°F (38°C) or higher.
- You experience severe breast pain that interferes with daily activities.
- You notice pus or blood in your breast milk.
- You feel a persistent lump in your breast that doesn’t go away after breastfeeding or pumping.
Questions to Ask the Doctor
Here are some questions you might want to ask your doctor if you have mastitis:
- What is the likely cause of my mastitis?
- Is the medication safe for my baby if I am breastfeeding?
- Can I continue breastfeeding or pumping? Is it recommended?
- Are there any home care measures I should continue to do?
- How can I prevent mastitis from recurring?
FAQs
1. Why are you getting mastitis more often?
If you experience the problem often, then there is a probability that you haven’t recovered completely from the condition. You are also prone to mastitis if you are weary or stressed. Hence, make sure the treatment is not delayed after you discover it for the second time. This is because the infection could cause an abscess in the breast and call for surgery.
2. Does having mastitis increase my risk of breast cancer?
Generally, having mastitis does not increase your risk of developing breast cancer. Mastitis is primarily an inflammatory or infectious condition. However, a rare type of breast cancer called inflammatory breast cancer can sometimes present with symptoms that mimic mastitis, such as redness, swelling, and warmth of the breast. Therefore, if mastitis symptoms don’t improve with treatment or if there are unusual or persistent changes in the breast, further investigation by a healthcare professional is crucial to rule out other conditions.
3. Can stress or lifestyle factors contribute to mastitis?
While the direct causes of mastitis are usually milk stasis or bacterial infection, indirect factors like stress, fatigue, and a weakened immune system can potentially increase the susceptibility to developing the condition, particularly lactational mastitis. Stress can interfere with milk let-down and efficient breastfeeding, potentially leading to milk stasis. Similarly, a compromised immune system might make it harder for the body to fight off bacteria that enter the breast. Maintaining a healthy lifestyle with adequate rest, proper nutrition, and stress management can be a supportive measure in preventing recurrent episodes of mastitis.
This was all about mastitis and breastfeeding. This is again a temporary phase and will fade away with time. But don’t ignore the symptoms and take the necessary precautions mentioned above to avoid the condition.
References/Resources:
3. National Library of Medicine – Acute Mastitis
4. Health Link BC – Mastitis While Breastfeeding
5. Cleveland Clinic – Mastitis
6. American Academy of Pediatrics – Mastitis: What Breastfeeding Parents Need to Know
Also Read:
Thrush while Breastfeeding
Causes of Breastfeeding Pain
Itchy Breast during Breastfeeding
Common Breastfeeding Problems and its Solutions
Was This Article Helpful?
Parenting is a huge responsibility, for you as a caregiver, but also for us as a parenting content platform. We understand that and take our responsibility of creating credible content seriously. FirstCry Parenting articles are written and published only after extensive research using factually sound references to deliver quality content that is accurate, validated by experts, and completely reliable. To understand how we go about creating content that is credible, read our editorial policy here.