Guillain-Barre Syndrome (GBS) in Children – Symptoms, Causes and Treatment

Imagine waking up to see your enthusiastic, playful child suddenly struggling to walk or complaining of unusual weakness. This can be scary and confusing as a parent, especially if it seems to come out of nowhere. How could this happen? What could be wrong? For many parents, this is the frightening reality of Guillain-Barre Syndrome (GBS). This rare condition can cause sudden weakness and even temporary paralysis, making it crucial for parents to know what to look for.
In this article, we’ll look at the mystery of Guillain-Barre Syndrome in children. What causes it? What warning signs should parents look out for? And most importantly, what treatments are available for GBS in infants? Please stick with us as we break it all down step by step, making sure you have the information you need to face this challenge head-on.
Expert Says
“GBS, when diagnosed on time and treatment started early, has full recovery. So keep a watch and reach out to your doctor early.”
– Dr. Gunjan Baweja
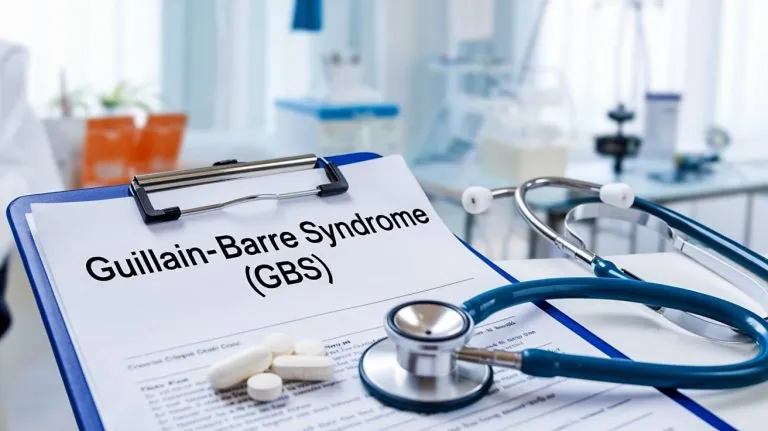
What Is Guillain-Barre Syndrome (GBS)?
Guillain-Barre Syndrome (GBS) is a rare autoimmune disorder in which the immune system mistakenly attacks the peripheral nervous system, the network of nerves outside the brain and spinal cord. The condition often develops rapidly and can cause muscle weakness, numbness, and, in severe cases, paralysis (1).
Types of Guillain-Barre Syndrome in Children
There are different types of GBS, each with unique characteristics that can affect how it develops and how it is treated. Let us take a closer look at the main types to understand them better (2).
1. Acute Inflammatory Demyelinating Polyneuropathy (AIDP)
This is the most common form of GBS in children. It happens when the body’s immune system attacks the myelin sheath, the protective covering of nerves, causing weakness, tingling, and sometimes difficulty moving.
2. Acute Motor Axonal Neuropathy (AMAN)
AMAN is a type of Guillain-Barre Syndrome that damages the axons of motor nerves, which are responsible for controlling muscle movements. This leads to sudden weakness or paralysis without affecting sensation, like numbness or tingling. It is seen more often in some parts of the world, like Asia and Central America.
3. Miller Fisher Syndrome (MFS)
Miller-Fisher Syndrome is a rarer form of GBS. It mainly affects eye muscles, causes loss of reflexes, and leads to problems with balance and coordination (3).
Is GBS Common in Children?
Guillain-Barre Syndrome (GBS) is rare in children, affecting only about 1 to 2 kids per 100,000 each year worldwide. While it can happen at any age, it is most seen in children between 1 and 5 years old (4).
Which Children Are at Risk of GBS?
Some children are more likely to develop Guillain-Barré Syndrome than others. Here are the main factors that might make a child more vulnerable to GBS.
- Gender: Boys may have a slightly higher risk of developing GBS compared to girls (5).
- Infections:Children who have recently had a cold, respiratory infection, or virus (such as the flu) are at increased risk of developing GBS.
- Immunisations: Although extremely rare, certain vaccines may occasionally trigger GBS in children.
Causes of GBS in Children
Have you ever wondered what might cause a condition as mysterious as GBS in children? Below are some of the most common reasons for Guillain-Barre Syndrome in kids (6) (7):
- Infections (Viral or Bacterial): Many cases of GBS in children are preceded by an infection, most commonly viral infections like the flu or respiratory viruses (e.g., Epstein-Barr virus, Cytomegalovirus) or bacterial infections like Campylobacter jejuni.
- Vaccinations: Although rare, GBS can develop after certain vaccinations, including those for the flu. The risk remains low, but it is still monitored.
- Genetic Factors: A family history of autoimmune disorders might contribute to a child’s risk of developing GBS (8).
- Recent Surgery or Injury: In some cases, children who have recently undergone surgery or been injured may develop GBS afterward.
Signs and Symptoms of GBS in Children
GBS can be a frightening condition for parents, especially when it affects children. Since the symptoms can progress quickly, it is important to recognize the warning signs early. Check the list below for common GBS infant symptoms, and if you notice any of the following signs, reach out to a doctor right away (1) (9).
1. Muscle Weakness
Muscle weakness, usually starting in the legs and spreading upwards, is one of the first signs of GBS. This weakness may make it difficult for the child to walk or stand.
2. Loss of Reflexes
Children with GBS may experience reduced or absent reflexes, particularly in the knees and ankles, leading to impaired movement and coordination.
3. Tingling or Numbness
A child may report tingling or numbness in their hands and feet, which can progress to other body parts.
4. Difficulty Breathing
In severe cases, GBS can affect the muscles involved in breathing, leading to shortness of breath or respiratory distress.
5. Facial Weakness
Facial muscles can also be affected by GBS, which may make it hard for your child to smile, eat, or speak clearly.
Complications of Guillain-Barre Syndrome in Children
Guillain-Barre Syndrome can be tough for children, not just because of the symptoms but also because of the complications it may cause. It can sometimes affect the autonomic nervous system, which controls vital functions like heart rate, blood pressure, and digestion. When GBS interferes with these automatic processes, it can lead to serious and life-threatening complications. Some of the most common issues that may arise include (1):
- Cardiac arrhythmias
- Unstable blood pressure
- Gastrointestinal issues
- Bladder control issues
Are There Any Long-Term Concerns?
For most children, Guillain-Barré Syndrome is a temporary challenge, and they recover fully with time and proper care. However, some may face lingering issues such as weakness, fatigue, or difficulty with coordination that can persist for months or even years. It’s also tough emotionally, especially when a child must rely on others for everyday tasks (10). The good news is that with consistent follow-up care and rehabilitation, many children overcome these hurdles and lead active, healthy lives.
How Is GBS in Children Different from Adults?
GBS affects both children and adults, but there are some important differences in how it impacts each group. The symptoms of GBS in children are very similar to those in adults, including weakness, tingling sensations, and muscle pain. However, in children, these symptoms often start in the legs and then spread to the upper body, making it difficult to walk or move their arms.
Adults may experience these symptoms as well, but sometimes, the symptoms can be more severe, affecting their ability to breathe and requiring immediate medical care. Children tend to have a somewhat lower risk of developing severe breathing problems (4), though they still need medical attention as GBS can progress quickly.
One of the biggest differences is recovery. Children often start to improve within weeks of treatment, while adults may take months or even years to fully recover. GBS is serious for both children and adults, but kids usually have a better chance of recovering (4).
Diagnosis of GBS in Children
Diagnosing Guillain-Barre Syndrome (GBS) in children can be tricky because it is a rare condition with symptoms that can easily be mistaken for other illnesses. Here’s a look at the main steps involved in the diagnosis of GBS in kids (9) (10):
1. Physical Examination
A thorough physical examination is essential to assess the strength of the child’s muscles, reflexes, and coordination. The doctor will test for any signs of muscle weakness or difficulty with movement.
2. Nerve Conduction Studies (NCS)
This test measures how well the nerves are sending signals to the muscles. In children with GBS, the nerve signals may be slower than usual, indicating nerve damage.
3. Lumbar Puncture (Spinal Tap)
A lumbar puncture involves taking a small sample of cerebrospinal fluid (CSF) from the spinal cord to check for abnormalities. In GBS cases, the CSF may show elevated protein levels without an increase in white blood cells.
4. Blood Tests
While there is no specific blood test for GBS, blood tests can help rule out other conditions with similar symptoms, such as infections or autoimmune disorders.
5. MRI
MRI scans can be useful in ruling out conditions that may present with similar symptoms, such as spinal cord issues or other neurological disorders.
How Is Guillain-Barre Syndrome Treated?
When a child is diagnosed with GBS, it is natural for parents to feel concerned about what comes next. While there is no cure, the good news is that effective treatments for Guillain-Barre Syndrome are available to manage symptoms and support recovery. Here are a few of the treatment options that doctors use to help children through this challenging condition (11) (12) (13):
- Intravenous Immunoglobulin: IVIg is one of the most common treatments for GBS. It involves administering antibodies from healthy blood donors through an intravenous (IV) infusion. This helps reduce inflammation and blocks the harmful antibodies attacking the nerves.
- Plasma Exchange (Plasmapheresis): This procedure removes harmful antibodies from the bloodstream that are attacking the nervous system.
- Pain Management: Medications are given to ease nerve pain or discomfort, which is common in children with GBS.
- Physical Therapy: Gentle exercises and therapy help rebuild strength, improve coordination, and speed up recovery.
- Breathing Support: In severe cases, ventilators may be used to help children breathe if their chest muscles are affected.
How Long Does It Take for a Child to Recover From GBS?
Recovery from Guillain-Barre Syndrome takes time and is different for every child. Children often show signs of improvement within 2 to 4 weeks after treatment, but it can take several months to a year for a full recovery (14). The good news is that children usually bounce back better.
Can Guillain-Barre Syndrome Be Prevented in Children?
Guillain-Barré Syndrome (GBS) is a rare condition, and unfortunately, it is not always preventable. While there is no guaranteed way to prevent GBS in children, there are a few steps that can help reduce the risk (1).
- Wash your hands regularly, as it helps reduce the spread of infections.
- Stay away from people who have infections, especially the stomach flu or respiratory illnesses.
- Eating a balanced diet and exercising can strengthen the immune system, helping to fight off infections.
- Ensure your child is up-to-datewith vaccinations.
When to Consult a doctor?
It is important to consult a doctor if you notice any signs or symptoms of Guillain-Barré Syndrome (GBS) in your child. Early intervention can make a big difference in treatment and recovery. You should seek medical help if:
- Your child experiences sudden weakness or tingling in their legs or arms.
- They have trouble walking or moving their body as usual.
- They feel numbness or a loss of sensation in any part of their body.
- Your child has difficulty breathing, swallowing, or speaking clearly.
FAQs
1. Is GBS contagious?
No, GBS is not contagious. It is an autoimmune condition, meaning the body’s immune system mistakenly attacks its own nerves (7).
2. Can Guillain-Barré Syndrome (GBS) occur in newborns?
GBS in newborns is extremely rare but can occur in exceptional cases. It is often triggered by factors such as maternal infections, perinatal infections, or, in rare cases, recent vaccinations (15).
3. How can parents support a child recovering from GBS?
Supporting your child emotionally, keeping up with doctor visits, and helping them with physical therapy can make a big difference in their recovery. Encouragement and a positive atmosphere at home are important to help them rebuild their strength and confidence (9).
Guillain-Barré Syndrome can be a frightening diagnosis for children and their families, but the road to recovery is often successful with the right treatment and support. Most children go on to lead healthy, active lives, and with time, the challenges of GBS become a distant memory.
References/Resources:
1. Guillain-Barré Syndrome; Cleveland Clinic; https://my.clevelandclinic.org/health/diseases/15838-guillain-barre-syndrome
2. Guillain-Barré Syndrome; Boston Children’s Hospital; https://www.childrenshospital.org/conditions/guillain-barre-syndrome
3. Cabrero. F. R, Morrison. E. H; Miller Fisher Syndrome; National Library of Medicine; https://www.ncbi.nlm.nih.gov/books/NBK507717/
4. Nasiri. J, Ghazavi. M, Yaghini. O, Chaldavi. M; Clinical Features and Outcome of Guillain-Barré Syndrome in Children; PubMed Central; https://pmc.ncbi.nlm.nih.gov/articles/PMC5904738/
5. McCombe. P. A, Hardy. T. A, Nona. R. J, Greer. J. M; Sex differences in Guillain Barré syndrome, chronic inflammatory demyelinating polyradiculoneuropathy, and experimental autoimmune neuritis; PubMed Central; https://pmc.ncbi.nlm.nih.gov/articles/PMC9780466/
6. Guillain-Barré Syndrome in Children; Cedars-Sinai; https://www.cedars-sinai.org/health-library/diseases-and-conditions—pediatrics/g/guillain-barre-syndrome-in-children.html
7. Guillain-Barré Syndrome; Centers for Disease Control and Prevention; https://www.cdc.gov/campylobacter/signs-symptoms/guillain-barre-syndrome.html
8. Khanmohammadi. S, Malekpour. M, Jabbari. P, Rezaei. N; Genetic basis of Guillain-Barre syndrome; PubMed; https://pubmed.ncbi.nlm.nih.gov/34246981/
9. Guillain-Barré Syndrome; Nemours KidsHealth; https://kidshealth.org/en/parents/gbs.html
10. National Institutes of Health; Guillain-Barré Syndrome; https://www.ninds.nih.gov/health-information/disorders/guillain-barre-syndrome#toc-how-is-guillain-barr-syndrome-diagnosed-and-treated-
11. Guillain-Barre Syndrome in Children; Children’s Hospital of Philadelphia; https://www.chop.edu/conditions-diseases/guillain-barre-syndrome-children#treatment
12. Guillain-Barré Syndrome; The Johns Hopkins Medicine; https://www.hopkinsmedicine.org/health/conditions-and-diseases/guillainbarr-syndrome
13. Guillain-Barré syndrome; NHS; https://www.nhs.uk/conditions/guillain-barre-syndrome/
14. When Your Child Has Guillain-Barré Syndrome (GBS); Saint Luke’s; https://www.saintlukeskc.org/health-library/when-your-child-has-guillain-barre-syndrome-gbs
15. Meshram. R. M, Bhongade. S. D, Gajimwar. V. S; Guillain Barre Syndrome: A Rare Cause of Floppy Neonate; PubMed Central; https://pmc.ncbi.nlm.nih.gov/articles/PMC7900717/
Also Read:
Chandipura Virus
Cold vs Flu in Children
Dengue Fever in Kids
Malaria in Children
West Nile Virus in Kids
Chikungunya in Children
Reye’s Syndrome in Children
Zika Virus Infection in Children
Was This Article Helpful?
Parenting is a huge responsibility, for you as a caregiver, but also for us as a parenting content platform. We understand that and take our responsibility of creating credible content seriously. FirstCry Parenting articles are written and published only after extensive research using factually sound references to deliver quality content that is accurate, validated by experts, and completely reliable. To understand how we go about creating content that is credible, read our editorial policy here.













.svg)